Understanding Diabetic Foot Ulcer Prevention and Treatment
Introduction
Diabetic foot ulcers are open sores or wounds that occur on the feet of individuals with diabetes. These ulcers are a significant concern as they can lead to severe infections, amputations, and even life-threatening complications if left untreated. Proper diabetic foot ulcer prevention and treatment are crucial for maintaining foot health and overall well-being in people with diabetes.
What Causes Diabetic Foot Ulcers?

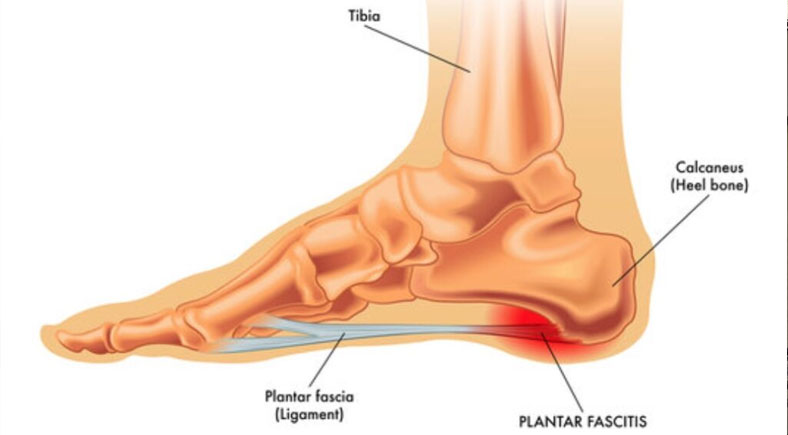
Diabetic foot ulcer develop due to a combination of factors linked to diabetes. Poor circulation, a common complication of diabetes, reduces blood flow to the feet, making it harder for wounds to heal. Nerve damage, or neuropathy, further compounds the issue by diminishing sensation in the feet, which may prevent individuals from noticing injuries. Minor cuts, blisters, or pressure points can easily progress into ulcer without prompt care. Foot deformities and ill-fitting shoes can also contribute to the development of these wounds.
Preventing Diabetic Foot Ulcers
The prevention of diabetic foot wounds is achievable through diligent foot care practices. Here are some effective diabetic foot care tips.
1. Daily Inspections
Daily foot inspections are vital for maintaining foot health, especially for individuals with diabetes or circulation issues. Check your feet every day for cuts, blisters, redness, swelling, or any unusual changes. Use a mirror to inspect hard-to-see areas or ask for assistance if needed. Early detection of issues helps prevent complications like infections or foot ulcer. Prioritize this simple yet essential step to protect your foot health.
2. Proper Footwear
Proper footwear is essential for maintaining healthy feet and preventing injuries. Always choose shoes that fit comfortably and provide ample support for your arches and heels. Avoid wearing tight or poorly fitted shoes that can cause blisters or pressure sores. Never walk barefoot, as this increases the risk of cuts, punctures, or infections. Prioritize protective footwear to keep your feet safe and healthy.
3. Blood Sugar Control
Maintaining optimal blood sugar levels is crucial for promoting healthy circulation and reducing the risk of foot-related complications, especially for individuals with diabetes. High blood sugar can damage nerves and blood vessels, leading to decreased sensation and slower healing. By managing your blood sugar through a balanced diet, regular exercise, and medication, you can protect your feet and overall health effectively.
4. Regular Moisturizing
Regular moisturizing is key to keeping your feet soft and preventing dry, cracked skin, which can lead to infections. Use a quality foot lotion or cream daily to maintain hydration, focusing on the tops and soles of your feet. However, avoid applying moisturizer between your toes, as excess moisture in this area can create an environment for fungal growth. Keep your feet healthy and protected with proper hydration care.
5. Routine Check-ups
Routine check-ups with a healthcare provider are essential for maintaining foot health, especially for individuals at higher risk of foot issues. Regular professional assessments can identify potential problems early, such as poor circulation, nerve damage, or skin conditions. Your healthcare provider can offer personalized advice and preventive care to keep your feet in optimal condition. Prioritize these check-ups as part of your overall health routine.
Treatment Options for Diabetic Foot Ulcers

Treatment options for diabetic foot ulcers focus on early intervention to prevent complications and promote healing. These may include regular wound cleaning and dressing changes to maintain hygiene, debridement to remove dead or infected tissue, and antibiotics to address infections. Advanced treatments, such as hyperbaric oxygen therapy or skin grafts, may be recommended for severe cases. Customized care plans and close medical supervision are essential for effective management.
1. Home Care
Proper home care is vital for effective wound management and healing. Clean the wound daily using mild soap and water to remove debris and reduce the risk of infection. After cleaning, apply an appropriate dressing that promotes healing while protecting the area. Avoid putting pressure on the affected site to prevent further irritation or delay in recovery. Consistent care ensures faster healing and helps prevent complications.
2. Medical Treatment
Medical treatment is essential for managing wounds effectively and preventing complications. Consult a healthcare professional for debridement to remove dead or infected tissue, promoting faster healing. They may prescribe antibiotics to combat infections and recommend specialized dressings tailored to your wound type for optimal recovery. Prompt professional care is crucial for ensuring proper wound management and minimizing risks.
3. Advanced Therapies
Advanced therapies are often recommended for severe or non-healing ulcers to promote recovery. Hyperbaric oxygen therapy enhances wound healing by improving oxygen supply to damaged tissues, while skin grafts can help repair and close persistent wounds. These specialized treatments are typically used under medical supervision for cases that do not respond to conventional care, offering hope for improved healing and better outcomes.
Timely treatment is essential to prevent complications such as infections or amputations. A healthcare provider will tailor the treatment plan to the severity and specific needs of the individual.
Conclusion
Diabetic foot ulcer are a serious condition that demands proactive prevention and effective treatment. By understanding the causes, implementing diabetic foot care tips, and seeking timely medical attention, individuals with diabetes can significantly reduce their risk of complications. If you or a loved one are dealing with diabetic foot ulcers, don’t wait—book a consultation today to explore effective diabetic wound care solutions.