Understanding Pressure Ulcers and How to Prevent Them
Introduction to Pressure Ulcers Causes and Prevention
Pressure ulcers causes and prevention are critical aspects of maintaining skin health, especially for individuals with limited mobility. Learn more about our specialized Pressure Ulcer Treatment Services designed to provide comprehensive care for managing and healing pressure wounds. Also known as bedsores, these localized injuries occur due to prolonged pressure on specific body areas, affecting the skin and underlying tissues. These wounds can severely impact overall health and quality of life, particularly for those who are bedridden, use wheelchairs, or have restricted movement. Proper understanding and proactive care are essential to prevent and manage pressure ulcers effectively. individual’s who are bedridden, wheelchair-bound, or otherwise immobile. Proper understanding and proactive care are essential to prevent and manage pressure ulcers effectively.
What Are Pressure Ulcers?
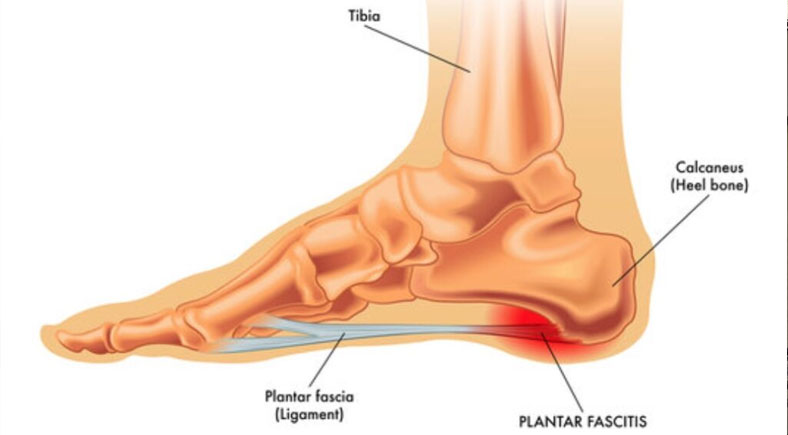
Pressure ulcers develop when consistent pressure reduces blood flow to certain areas of the body, causing tissue damage. Individuals at risk should consider scheduling a Regular Foot Exam to detect early warning signs and prevent complications. Common sites for these wounds include bony prominences like the heels, ankles, hips, and tailbone. When the skin and underlying tissues are deprived of oxygen and nutrients for an extended period, they break down, resulting in sores that can range from mild redness to deep wounds exposing muscles and bones.
For individuals with limited mobility, such as those with disabilities or chronic illness, pressure ulcers can form quickly and become severe without timely intervention.
Causes and Prevention of Pressure Ulcers
What are the Factors Causes Pressure Ulcers?
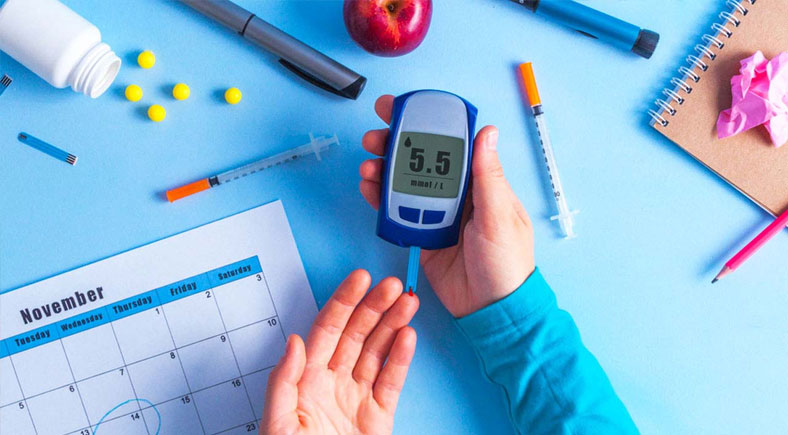
Several factors increase the risk of developing pressure ulcers, including immobility, poor circulation, and inadequate foot care. For professional guidance, check out our Diabetic Ulcer Treatment to understand how proper wound care can prevent severe complications.
1. Immobility: Extended periods of lying or sitting in the same position create sustained pressure on specific areas, leading to reduced blood flow and oxygen delivery to the skin and tissues, increasing the likelihood of ulcer formation.
2. Diabetes: Poor circulation and nerve damage associated with diabetes make the skin more vulnerable to injury, slow the healing process, and heighten the risk of infections, further complicating the condition.
3. Poor Nutrition: Lack of essential nutrients like protein, vitamins, and minerals weakens the skin’s ability to repair itself and fight infections, making it more prone to breakdown under pressure or friction.
4. Incontinence: Prolonged exposure to moisture from urine or feces irritates the skin, breaking down its natural barrier, while bacteria in waste increase the chances of infection and ulceration.
5. Advanced Age: Older adults often have thinner, less elastic skin with diminished blood supply, making them more prone to pressure-related injuries and slower recovery.
6. Medical Conditions: Conditions such as peripheral artery disease and chronic illnesses affect blood circulation and skin integrity, reducing the skin’s resilience and increasing susceptibility to pressure ulcers.
How to Prevent Pressure Ulcers

Preventing pressure ulcers requires a proactive approach that addresses the risk factors and promotes skin health. Discover expert Wound Prevention Techniques that focus on skin protection, early intervention, and advanced wound care.
1. Repositioning: Encourage regular movement and repositioning to relieve pressure on vulnerable areas. For bedridden individuals, this may mean turning every two hours to improve blood flow, prevent skin breakdown, and reduce prolonged pressure on bony areas like hips and heels.
2. Specialized Equipment: Use pressure-relieving mattresses, cushions, and heel protectors to distribute weight more evenly and reduce pressure on specific points. Equipment like alternating air mattresses and foam cushions can significantly lower the risk of developing sores.
3. Proper Foot Care: Maintain clean, dry feet, especially for individuals with diabetes, to reduce the risk of sores. Daily inspection for redness, blisters, or skin changes ensures early intervention and prevents complications from unnoticed injuries.
4. Skin Protection: Apply moisturizers to keep the skin hydrated and use barrier creams to prevent irritation from moisture caused by incontinence or excessive sweating. Avoid harsh soaps that can strip natural oils and compromise skin integrity.
5. Nutrition and Hydration: Ensure a diet rich in protein, vitamins (like Vitamin C), and minerals (like zinc) to support skin integrity and wound healing. Proper hydration also enhances blood circulation, which is essential for maintaining healthy skin.
Hygiene: Keep the skin clean and dry, especially in areas prone to sweating or incontinence. Frequent cleaning with gentle products and patting the skin dry prevents irritation and infection.
6. Regular Monitoring: Caregivers should routinely check for redness, swelling, or other early signs of pressure ulcers to address them before they worsen. Frequent monitoring ensures timely treatment and reduces the chances of ulcer progression.
Conclusion
Preventing pressure ulcers is crucial for maintaining the health and comfort of individuals at risk. If you or a loved one needs specialized care, our Comprehensive Wound Care Services provide expert treatment for various foot conditions, including pressure ulcers, venous ulcers, and diabetic wounds. By incorporating strategies like repositioning, using specialized equipment, and ensuring proper nutrition and hygiene, caregivers can significantly reduce the likelihood of these painful wounds. Regular monitoring and early intervention are key to effective pressure ulcer care, ensuring a better quality of life for those affected. Prioritize wound prevention tips and proper care to stay ahead in preventing bedsores.